Prenatal genetic diagnosis
Prenatal genetic diagnosis
Unimed prenatal genetic diagnosis is a technology that uses microarray chips to detect amniotic fluid, villus or umbilical cord blood samples to diagnose fetal congenital defects and hereditary diseases.
Prenatal diagnosis is different from prenatal screening. Prenatal diagnosis is one of the most accurate methods of troubleshooting. Among them, the amniotic fluid puncture technique is the most widely used. If Down's screening shows high risk, it is still recommended that prospective mothers have an amniotic fluid puncture examination. Amniotic fluid puncture is still the "gold standard" for prenatal diagnosis.
Prenatal diagnosis method
Prenatal genetic diagnosis, also called intrauterine diagnosis, refers to the diagnosis of fetal birth defects before birth. The main prenatal diagnosis methods are: amniocentesis, villus sampling, and umbilical cord puncture.
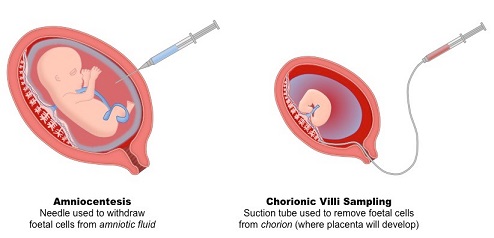
1. Amniocentesis: It is the most widely used technique in prenatal diagnosis. Generally, it is carried out at 16-20 weeks of pregnancy. At this time, there is more amniotic fluid and the fetus is small. There is a wide layer of amniotic fluid around the fetus. The proportion of cells is also the highest, and the culture survival rate is high. Amniocentesis is generally performed aseptically in an outpatient setting. After urination, the pregnant woman is supine and disinfected. Under ultrasound guidance, use a 20-22 lumbar puncture needle to reach the amniotic cavity through the abdominal wall and myometrium, and then extract 15-20ml amniotic fluid for culture. The entire process is about 5-10 minutes. The risk of post-abortion is about 0.3%.
2. Villus sampling: Generally performed at 8-10 weeks of pregnancy under ultrasound guidance. Generally, 5-10 mg of villi near the implantation site of the embryo are sucked and immediately sent to the laboratory for culture. Aspiration of such a small amount of villi will not affect placental function, but may cause miscarriage, rupture of the membranes, bleeding at the villi, intrauterine infection, amnion band syndrome, and sensitization of Rh blood group. Compared with amniocentesis, the biggest advantage of villous sampling is that the material is collected early, and high-risk pregnant women do not have to endure the long-term suffering. Puncture is much higher.
3. Umbilical cord puncture: generally performed at 18 weeks of pregnancy. Under ultrasound guidance, a 20-22 lumbar puncture needle is inserted into the umbilical cord through the abdominal wall to obtain blood. Fetal blood can be diagnosed: (1) blood diseases, such as hemoglobinopathy , Thrombocytopenia, and abnormal coagulation factors; (2) congenital metabolic diseases; (3) viral, bacterial, and other microbial infections; (4) fetal blood cytogenetics when chromosomes are chimeric in villi or amniotic fluid culture It can be identified whether a chimera really exists. When performing cytogenetic examinations, results can be obtained in 48-72 hours with short-term fetal lymphocyte cultures. Umbilical cord puncture has a higher risk of miscarriage than amniocentesis, and may also cause complications such as umbilical cord bleeding, intrauterine death, infection, premature birth, and RH blood group sensitization, so unless a rapid diagnosis is needed, or other safer Use this technique only if your prenatal diagnostic method does not give satisfactory results.
Sample requirements
• Amniotic fluid: Collect 5 ~ 10ml, place in screw-top centrifuge tube, and store at 4 ℃;
• Villi: take the size of soybean, rinse twice with sterile solution or normal saline, put it in EP tube, and store at 4 ℃;
• Umbilical cord blood: Collect 1 ~ 2ml, put it in EDTA tube, and store at 4 ℃;
